Back Pain
Have you ever been down in your back? If not there’s a pretty good chance you will be at some point in your life. It may be as simple as a dull annoying sensation, or the pain can be temporarily debilitating to the point that it is difficult to perform simple daily activities and impossible to go to work.
According to the National Institute of Neurological Disorders and Stroke, Americans spend at least $50 billion each year treating low back pain. Back pain is the most common cause of job related disabilities, and it is one of the main reasons people miss work.
 One factor related to the development of chronic low back pain (back pain lasting more than 3 months) is a lack of strength in the muscles that support the lumbar spine (Pollock et al., 1989).
One factor related to the development of chronic low back pain (back pain lasting more than 3 months) is a lack of strength in the muscles that support the lumbar spine (Pollock et al., 1989).
Your spinal column is the only boney connection you have between your upper and lower body. It is composed of 24 moveable vertebrae and 9 fused vertebrae (the sacrum and the coccyx). The vertebrae contain your spinal column along with 31 pairs of spinal nerves that serve as the communication and command system between your body and your brain.
Between each moveable vertebra is a disc whose job is to act like a shock absorber, reducing the impact of stress in the column. Each disc is like a jelly donut with a soft center (nucleus pulposus) and a firm outer ring (annulus fibrosus) composed of compressed elastic material.
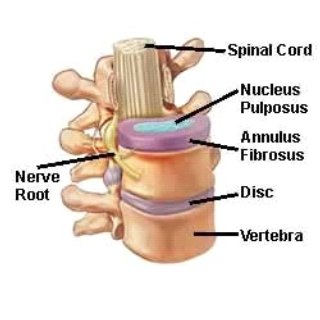 Several ligaments limit motion and help hold vertebrae together. Also, many small muscles connect vertebrae to vertebrae and help stabilize the spine while you are sitting in a chair or chasing your two-year old around the house.
Several ligaments limit motion and help hold vertebrae together. Also, many small muscles connect vertebrae to vertebrae and help stabilize the spine while you are sitting in a chair or chasing your two-year old around the house.
There is not a lot of movement possible between any 2 vertebrae. However, the cumulative effect of 24 moveable vertebrae, 23 spongy discs, numerous ligaments running up and down the spine, and muscles that span the entire back allows the spine to move in many directions, sort of like a snake.
So why is it so easy to injure your lower back? The lumber spine (the 5 moveable vertebrae that form that nice inward curvature in the lower part of your back) is under more stress because it supports more weight from your upper body. You often hear people say their back pain is “L4 – L5,” that’s because the 4th and 5th lumbar vertebrae are the lowest large vertebrae and the disc between these two has to support more upper body weight than any other disc.
Age, trauma, or improper use of the spine can cause the fibrous part of the disc to become weakened. When this happens compression of the spine can cause the jelly part of the disk (nucleus) to protrude through the fibrous part of the disk (annulus). This is what is commonly referred to as a herniated or slipped disk. The protruding nucleus can put pressure on a spinal nerve root causing a variety of symptoms, including radiating pain, tingling, numbness and weakness of the muscles innervated by the effected nerve.
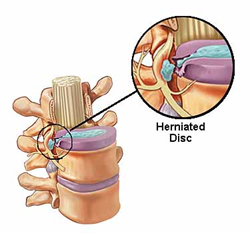 Many low back problems are caused by improper use of the back over time. This results in acute strains and muscles spasms, which cause mechanical changes that can lead to disk herniation. Most problems occur when you use the small back muscles to lift objects from a flexed spine position, instead of keeping the lumbar spine in a neutral position, while squatting and using the larger more powerful muscles of the legs.
Many low back problems are caused by improper use of the back over time. This results in acute strains and muscles spasms, which cause mechanical changes that can lead to disk herniation. Most problems occur when you use the small back muscles to lift objects from a flexed spine position, instead of keeping the lumbar spine in a neutral position, while squatting and using the larger more powerful muscles of the legs.
There are four factors that are essential to spine health:
- Strength
- Stability
- Flexibility
- Endurance
One factor related to the development of chronic low back pain is insufficient strength in the muscles that extend the lumbar spine (May & Donelson, 2008). Because of this, strength training is often prescribed for prevention and treatment of low back pain (Nelson et al., 1995).
At Exercise Inc we use the Medx Lumbar Extension (MedX, Ocala, FL), which is a unique back strength-training machine that will allow you to safely and efficiently improve all four factors of spine health.
The Medx Lumbar Extension is the only low back machine that has a patented, pelvic restraint system that stabilizes the pelvis and minimizes the contribution of the hip and leg muscles. It isolates the muscles of your lumbar spine, allowing them to become more involved in the exercise.
Check out this animation that shows the restraint system at work.
Used by permission of Serious Strength
Numerous studies have shown that just one exercise session a week on the Medx Lumbar Extension can produce significant increases in strength and decrease low back pain (Bruce-Low et al., 2012; Choi et al., 2005; Tucci, Carpenter, Pollock, Graves, & Leggett, 1992). Research has also shown that training more than once a week does not produce any greater improvements (Bruce-Low et al., 2012; Smith, Bruce-Low, & Bissell, 2008). So, one training session a week on our back machine will give you the best results.
Also, subjects in a study in 2012 reported that their pain had decreased after training once a week for 12 weeks on the MedX Lumbar Extention (Bruce-Low et al., 2012). In the same study the subjects significantly increased their flexibility. The data in this study and the other studies cited in this article support previous research that muscular pain is potentially the result of muscular weakness.
It has also been shown that using the MedX lumbar extension once a week can reduce the likelihood of injury in the workplace (Mooney, Kron, Rummerfield, & Holmes, 1995).
Finally, the last benefit I want to mention from using our MedX Lumbar Extension is spinal lubrication. Regular movement of the lumbar spine may help reduce the loss in hydration that occurs with aging of the disks (Norris, 2008). Discs that have reduced osmotic pressure (dryer disks) are more likely to crack and herniate. Movement on the MedX Lumbar Extension has the potential to increase disk hydration.
So to review what we just discussed. By training no more than once a week on our MedX Lumbar Extension, you can experience the following benefits:
- More Strength In Your Lumbar Spine
- Improved Flexibility In Your Back
- Decreased Back Pain
- Fewer Days Off From Work (Or Play) Due To Back Pain
- Increased Disk Hydration
- Reduced Risk of Injury
Stay Strong,
Bo Railey
Click the links below to see what our clients have to say about training once a week at Exercise Inc on the MedX Lumbar Extension.
Bruce-Low, S., Smith, D., Burnet, S., Fisher, J., Bissell, G., & Webster, L. (2012). One lumbar extension training session per week is sufficient for strength gains and reductions in pain in patients with chronic low back pain ergonomics. Ergonomics, 55(4), 500-507.
Choi, G., Raiturker, P. P., Kim, M. J., Chung, D. J., Chae, Y. S., & Lee, S. H. (2005). The effect of early isolated lumbar extension exercise program for patients with herniated disc undergoing lumbar discectomy. Neurosurgery, 57(4), 764-772; discussion 764-772.
May, S., & Donelson, R. (2008). Evidence-informed management of chronic low back pain with the McKenzie method. Spine J, 8(1), 134-141.
Mooney, V., Kron, M., Rummerfield, P., & Holmes, B. (1995). The effect of workplace based strengthening on low back injury rates: A case study in the strip mining industry. J Occup Rehabil, 5(3), 157-167.
Nelson, B., Hogan, M., O’Reilly, E., Wegner, J. A., Miller, M., & Kelly, C. (1995). The clinical effects of intensive specific exercise on chronic low back pain: A controlled study of 895 consecutive patients with 1-year follow up. Orthopedics, 18(10), 971 – 981.
Norris, C. M. (2008). Back stability: integrating science an therapy. Champaign, IL: Human Kinetics.
Pollock, M. L., Leggett, S. H., Graves, J. E., Jones, A., Fulton, M., & Cirulli, J. (1989). Effect of resistance training on lumbar extension strength. Am J Sports Med, 17(5), 624-629.
Smith, D., Bruce-Low, S., & Bissell, G. (2008). Twenty years of specific, isolated lumbar extension research: a review. Journal of Orthopaedics, 5(14).
Tucci, J. T., Carpenter, D. M., Pollock, M. L., Graves, J. E., & Leggett, S. H. (1992). Effect of reduced frequency of training and detraining on lumbar extension strength. Spine (Phila Pa 1976), 17(12), 1497-1501.



