Building Strong Bones
Strong bones are just as important to our health as strong muscles. It sounds odd to talk about bones being strong. Most of the bones we’ve ever seen seem like hard, lifeless structures—fixed to a shape and size that doesn’t seem to change past puberty. But that’s not the case.
Bones are a dynamic tissue matrix of collagen and minerals, like calcium and phosphorus. They exist in a continual state of flux called remodeling. As an adult, your body replaces the minerals in your skeleton every 10 years. And just like your muscles, you can train your bones to be strong.
Calcium
The most important developmental period for bone mass occurs in our early teen years. It’s extremely important to be physically active during those years and to get adequate calcium. The biggest factor affecting bone health—calcium availability. Teenagers need about 1300 mg of calcium a day, or the calcium in five 8-oz glasses of milk.
 Adults need about 1000 mg of calcium a day, but most adults only get 500 to 700 mg a day. Not getting enough calcium can compromise bone strength. Calcium plays a role in several major functions of your body including muscle contractions, nerve impulse transmissions, transport of fluids across cell membranes, and blood clotting. If your body isn’t getting enough calcium from your diet, it will withdraw calcium from your bones to restore the deficit. If this happens consistently over time, bones will become less mineralized and weaker.
Adults need about 1000 mg of calcium a day, but most adults only get 500 to 700 mg a day. Not getting enough calcium can compromise bone strength. Calcium plays a role in several major functions of your body including muscle contractions, nerve impulse transmissions, transport of fluids across cell membranes, and blood clotting. If your body isn’t getting enough calcium from your diet, it will withdraw calcium from your bones to restore the deficit. If this happens consistently over time, bones will become less mineralized and weaker.
Getting adequate calcium daily is critical to bone health. The best sources of calcium include milk and milk products, sardines, canned salmon (eat the bones), kidney beans, and dark green vegetables. Many people resort to calcium supplements, which do help, but the best source of calcium is calcium-rich foods.
Physical Activity
Mechanical loading through physical exercise builds strong bones during our youth and keeps them strong as we age. The most important time of life for bone growth is during childhood and adolescence when peak bone mass increases to its greatest extent. That’s why it’s extremely important for kids to be as active as possible.
But it’s also important to stay active to keep bones strong throughout your life. Bones operate on a “use it or lose it” principle. Wolff’s law, an anatomical rule that describes how bone grows and changes over time, states that the body adds bone where it is needed and removes it where it is not. Julius Wolff, a German surgeon, stated that if the body is involved in repeated activity, the skeleton will respond by becoming larger and stronger.
The opposite of that statement is true as well—if the body becomes sedentary, bones become smaller and weaker. That happens to a significant number of adults after age 50.
Low levels of physical activity combined with inadequate calcium intake can lead to one of two conditions—osteopenia or osteoporosis. Osteopenia, which literally means “bone poverty,” is a condition where bones weaken, increasing the risk of fracture.
Osteoporosis
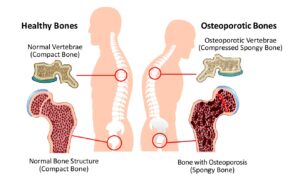
Osteoporosis, literally meaning “porous bones,” is a condition where bones deteriorate to the point that they become more brittle and porous (having minute spaces or holes). People with osteoporosis will often experience broken bones simply by coughing or bumping into something. They are more likely to break bones in their hip and spine. Sometimes the spine will break and collapse to the point that people get shorter and can’t stand up straight.
The most serious consequence of having osteoporosis is a broken bone in the hip. Many people who break their hip can’t live on their own and are more likely to die sooner. With osteoporosis, the hip can break spontaneously, resulting in a fall—the opposite of what should happen.
Osteoporosis affects 20% (1 in 5) of women and 5% (1 in 20) of men over age 50. One out of two women and one out of eight men can expect an osteoporosis-related fracture in their lifetime. Women comprise eighty percent of people with osteoporosis.
Estrogen
Women experience a greater risk of osteoporosis after menopause because of the marked decrease in estrogen. Most men naturally produce estrogen into old age because a portion of circulating testosterone converts to estrogen. Scientists struggled to unlock estrogen’s role in bone health until a recent study revealed estrogen is responsible for expression of a protein in bone cells (osteocytes) that promotes their survival. Estrogen also helps the intestines absorb calcium and reduces urinary calcium excretion.
Screening
Most people with osteoporosis don’t know they have it until they break a bone. That’s why screening for osteoporosis is important. Doctors recommend osteoporosis screening for women over 65 or postmenopausal women over 50 whose parent has broken a hip.
Doctors typically screen for osteoporosis with a DXA (dual-energy X-ray absorptiometry) scan, which measures bone mineral density at the spine, hip, or total body. A DXA scan test will give you a T-score, which compares your bone mineral density with what is normally expected in a healthy young adult. Your T-score is the number of units—called standard deviations—that your bone density is above or below the average. A T-score of -1 to -2.5 indicates osteopenia, which means your bone density is below normal and may lead to osteoporosis. A T-score below -2.5 indicates osteoporosis.
Treatment for osteoporosis usually involves a particular class of drugs called bisphosphonates. Fosamax, taken daily, weekly, or monthly, seems to be the most popular. Bisphosphonates strengthen bones by slowing the rate at which the body removes calcium. But, as with any drug, side effects can occur. Bisphosphonates can cause gastrointestinal problems such as trouble swallowing, inflammation of the esophagus, and ulcers.
If you have osteoporosis and your doctor puts you on prescription medication, stick to your doctor’s plan. But in addition to that, we recommend you do what you can to build strong bones on your own.
Strength Training
Extensive research shows Strength Training has a very positive affect on bone mineral density. It has even been proven to reverse osteoporosis. When you combine strength training with proper nutrition, some amazing changes can take place.

At Exercise Inc, we use the Super Slow method of strength training. The method was the result of an osteoporosis study conducted at the University of Florida in the 1980s. The study attempted to determine if strength training could prevent bone mineral loss in a group of women who were over 50, post-menopausal, and had osteoporosis.
The researchers found that these weak, frail women had trouble lifting weights at traditional speeds. They decided to have the women lift the weights very slowly (10 seconds up) to reduce the force of the exercises. This made the program safe enough for the women to perform the exercises. After about 12 weeks, these weak, frail women produced a 30 percent greater increase in strength than anything they’d seen in any other strength training studies.
In addition to making exercise safer, the Super Slow method also made it more productive. We have had a lot of success helping our clients prevent and reduce osteoporosis. We have featured several of those success stories on our Facebook page. You can find my favorite Exercise Inc osteoporosis success story in a blog post on our website about a client who reversed her osteoporosis diagnosis.
Melanie Sargent was diagnosed with osteoporosis at age 50. Her doctor prescribed Fosamax and recommended she start strength training. That was way back in 1999 when she started training with me at The Training Zone (before Exercise Inc). After 10 years of strength training combined with the drug Fosamax, Melanie’s doctor declared she no longer had osteoporosis, and her T-score confirmed her bone mineral density had returned to a healthy level. At age 74, Melanie continues to strength train at Exercise Inc. She is strong, healthy, has no back pain, and she can stand up straight.
A 2017 meta-analysis found that high intensity strength training provides the maximum benefit in increasing bone mineral density. When combined with adequate calcium intake, strength training will go a long way in making your bones strong.
If you or someone you know has osteoporosis (or hopes to prevent it), please send them our way for a free initial consultation.
Stay Strong,
Bo Railey

